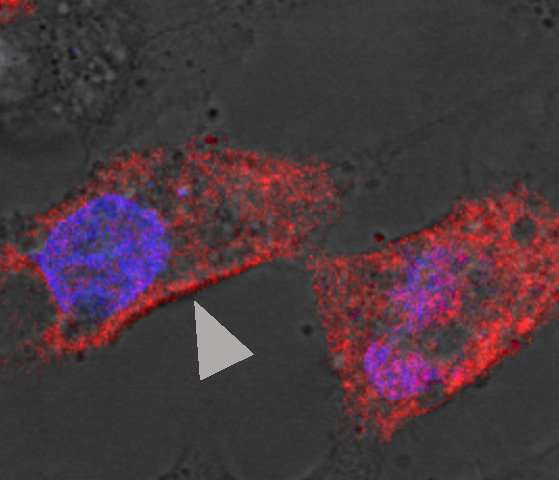
Hepatitis B core antigen (arrow head) on the cellular membrane in cells transfected with hepatitis B virus. The virus is derived from a patient with acute liver failure. Credit: NIAID
National Institutes of Health scientists and their collaborators found that hepatitis B virus (HBV)-associated acute liver failure (ALF)—a rare condition that can turn fatal within days without liver transplantation—results from an uncommon encounter between a highly mutated HBV variant and an unusual immune response in the patient’s liver that is mainly sustained by antibody-producing B cells.
By applying state-of-the-art technologies, the researchers discovered important new mechanisms about the disease by examining liver samples taken from four patients who developed HBV-ALF. HBV-ALF is one of the most dramatic clinical syndromes in medicine, according to the research team, but so rare that samples of this type are seldom available for study.
Scientists from NIH’s National Institute of Allergy and Infectious Diseases (NIAID) led the project with colleagues from two Italian universities. Their study is published in Proceedings of the National Academy of Sciences.
The investigators used advanced gene sequencing and tissue and cell analysis technologies to determine specific molecular events occurring at the site where HBV replicates and damages liver tissue. They identified processes that are distinct to HBV-ALF cases compared with cases of classic acute HBV infection. Some of these unique events involve a highly mutated virus antigen, the HBV core antigen. The scientists believe that this antigen plays a key role in disease development because it interacts with specific antibodies that are—unusually, they say—already present in these patients. Because of ethical reasons in obtaining liver tissues from patients with classic acute HBV, for their comparison study the scientists used archived liver specimens from two chimpanzees with acute HBV that had been studied many years earlier. They found the mechanism of acute HBV disease to be completely different from that of ALF.
According to the scientists, the HBV-ALF findings were consistent among samples taken from all four patients studied. That is important validation, they say, because virtually no studies have been done on the molecular pathogenesis of HBV-ALF in the liver. They hope their new work provides a model of how the disease develops and will lead to new diagnostic, treatment and prevention strategies.
Journal reference:
Proceedings of the National Academy of Sciences
Provided by:
NIH/National Institute of Allergy and Infectious Diseases